October 14, 2020 — Editor’s note: This story is part of a nine-month investigation of drinking water contamination across the U.S. The series is supported by funding from the Park Foundation and Water Foundation. View related stories here.
Before her 73-year-old mom contracted Legionnaires’ disease at a nursing home earlier this year, Monique Barlow knew little about the deadly pneumonia and the waterborne pathogen that causes it.
“Until then, I didn’t give it much thought,” says Barlow. “I didn’t even really know what it was.”
Sheryll Barlow, a resident of Room 325 at Arlington Court Skilled Nursing and Rehab Center in suburban Columbus, Ohio, died in late February. Arlington Court was just one of at least five Columbus-area facilities to report an outbreak of Legionnaires’ disease, which is caused by Legionella bacteria, since May 2019.
Modern drinking water treatment in developed countries has effectively eliminated cholera, typhoid and other traditional waterborne scourges. The U.S. Safe Drinking Water Act (SDWA), passed in 1974, propelled progress by requiring water suppliers to meet national standards for monitoring contaminants and managing them through filtration, disinfection and other processes. The U.S. now has one of the world’s safest drinking water supplies. And most of the attention on drinking water safety today has shifted from microbiological to chemical, with plastics, pesticides and per- and polyfluoroalkyl substances, or PFAS, leading lists of contaminants of concern.
 Yet many microorganisms also slip through the cracks of U.S. drinking water systems, sickening up to an estimated 4 million to 32 million people every year. Although most only result in mild gastrointestinal upsets, some can be deadly, as witnessed by recent reports of brain-eating amoeba in Texas municipal water supply.
Yet many microorganisms also slip through the cracks of U.S. drinking water systems, sickening up to an estimated 4 million to 32 million people every year. Although most only result in mild gastrointestinal upsets, some can be deadly, as witnessed by recent reports of brain-eating amoeba in Texas municipal water supply.
That figure doesn’t include wells, which are particularly prone to pathogen problems. In 2000, some 2,300 people fell ill and seven died in Walkerton, Ontario, for example, after heavy rainwater drew E. coli and Campylobacter jejuni bacteria from cow manure into a shallow aquifer of a nearby well.
Typical concentrations of chlorine used in treatment plants can be insufficient to kill off Cryptosporidum and Giardia, which cause gastrointestinal disease. And other infectious agents, including Legionella and non-tuberculosis mycobacteria, reside beyond the reaches of the treatment plant — finding hospitable environments in the pipes that distribute water to and within hospitals, hotels, homes and other buildings.
“It’s never going to be 100%, but we have things well under control for pathogens in source waters,” says Joe Cotruvo, an environmental and public health consultant based in Washington, D.C., and formerly with the U.S. Environmental Protection Agency’s Office of Drinking Water. “The data show that those risks are going down and have been going down ever since the Safe Drinking Water Act was implemented.”
That is, Cotruvo adds, with one exception. “What has been going up has been Legionella.” Figuring out why — and what do to about it — is a major focus of efforts to combat waterborne diseases today.
Attention to Legionella has been heightened by the Covid-19 pandemic. Some health experts express concern that a prior infection with the virus that causes Covid-19 could make a person more susceptible to Legionella. But there’s an even more pressing concern connecting the two: Building shut-downs through the spring and summer have left warm water stagnant in pipes — a perfect environment for Legionella to multiply.
Many hotels, offices, schools and other buildings have been left fully or partially vacant for long periods of time, notes Chris Edens, an epidemiologist with the U.S. Centers for Disease Control and Prevention (CDC), which recently released guidance for reopening buildings. “As those kinds of communities reopen, it’s important for owners and operators to be thinking about water management.”
Leading Cause
Legionella grows naturally in the environment, especially warm freshwater lakes and streams that can be a source for drinking water. It generally only becomes a risk to human health when it enters and multiplies within human-made water and plumbing systems, and then that contaminated water becomes aerosolized.
Drinking fountains, hot tubs, sinks, toilets, sprinklers, showers and air-conditioning systems are among the common sources. It tends to flourish when temperatures are warm, water is stagnant, chemical disinfectants are insufficient, and nutrients are plentiful, such as inside corroding pipes. When inhaled at high enough levels, the bacteria can infiltrate the lungs and cause one of two forms of legionellosis, Pontiac fever or Legionnaires’ disease. The former is usually a fairly mild respiratory illness; the latter is far more commonly reported and estimated to be fatal in one in 10 cases.
Now the leading cause of reported waterborne disease in the U.S., Legionella accounts for about 60% of outbreaks over the last decade. Nearly 10,000 cases of Legionnaires’ disease were reported to the CDC in 2018 — the most ever in U.S. history, and still a likely underestimate. Edens suggests the true figure is probably double that. Other scientists estimate the annual case count at between 52,000 and 70,000.
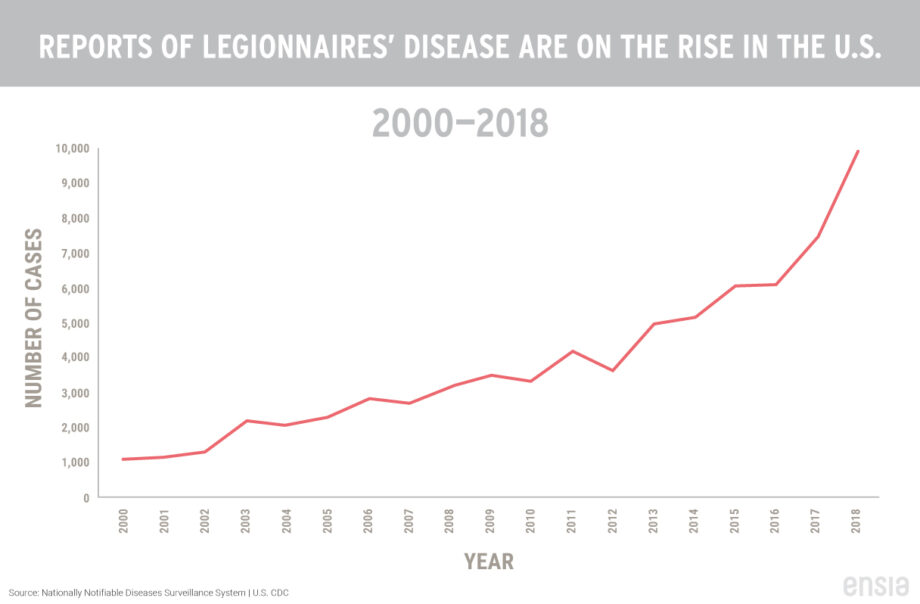
Reports of Legionnaires’ disease have climbed in recent years. No one is sure why, but factors could include improved reporting, aging people and infrastructure, and climate change. Click image to expand.
Legionnaires’ disease was discovered in 1976 after some 200 people became ill with a mysterious type of pneumonia-like disease at an American Legion convention in Philadelphia. Dozens died. Health officials eventually identified a bacterium that had thrived in the building’s cooling towers and then spread though the air-conditioning system.
Cooling towers were also likely behind many of the more than 2,000 confirmed cases in New York City between 2006 and 2015. In the summer of 2019, the Sheraton Atlanta hotel was closed for a month after an estimated 79 people were infected from Legionella traced to the hotel’s cooling tower and decorative fountain. A variety of other plumbing issues and insufficient water management has resulted in outbreaks around the country — at nursing homes, hospitals, schools and across whole communities.
At least 87 people were infected with Legionnaires’ disease in Flint, Michigan, in 2014 and 2015 after the city switched water sources. Researchers found evidence for three likely sources of Legionella exposure: a hospital, City of Flint water and local cooling towers. Mayor Sheldon Neeley told Ensia that the city is “making critically important infrastructure improvements to move our community forward in a positive direction.”
Proliferating Pathogen
Yet such large-scale Legionnaires’ disease outbreaks are “just the tip of the iceberg,” according to Joan Rose, a water researcher at Michigan State University. Research suggests that for every case linked to a specific source and outbreak there are nine sporadic cases. For example, outbreaks only accounted for about 10% of the cases in New York City linked to cooling towers.
“We don’t have Legionella under control,” says Rose.
Why does Legionella appear to be on the rise around the U.S.? The answer is complicated, explains Edens. The larger numbers could be partly due to greater awareness and testing. But he suggests that an aging population and aging infrastructure are major drivers.

Legionella tends to flourish when temperatures are warm, water is stagnant, chemical disinfectants are insufficient and nutrients are plentiful, such as inside corroding pipes. Photo courtesy of cattalin from pixabay.com
“In large part, our distribution system is very antiquated,” says Amy Pruden, a professor of civil and environmental engineering at Virginia Tech. As water travels through the distribution system and enters a building, it can lose disinfectant as well as interact with the materials, temperatures and design of the building’s plumbing. “Many things are at play that affect whether these microbes grow in the plumbing,” she adds.
Climate change, too, may be playing a role. Longer summers tax the cooling devices used by large buildings. Increased rainfall may increase the presence of Legionella in drinking water.
It’s all added up to growing concerns and heightened calls to address the risks. “The thing about Legionella is it’s a silent killer. You can’t see it or smell it. It’s just in the air floating around,” says Eric Hageman, a Minneapolis lawyer who represents the family of Sheryll Barlow in a claim against Arlington Court. “So, you have to be proactive.”
Controlling Contaminants
Arlington Court had been aware of a Legionella problem at the facility months before Monique Barlow’s mom became sick after another resident contracted Legionnaires’ disease in October 2019. “I just assumed they took care of everything. But then it popped back up, and that’s when we got the call,” says Barlow.
After learning that her mom had the disease, she says she wanted to know more. “I felt like they owed us an explanation. How are you fixing this? How is this not going to happen again?” Barlow adds.
Since February 10, Arlington Court has implemented changes, including the installation of filters in the kitchen, visitor areas, showers, bathrooms and ice machines. Such point-of-use filters are among emerging tools to control Legionella.
In a letter to residents reported on March 1 after local officials announced an investigation of an outbreak, Arlington Court said it took “very seriously the health and safety of everyone at the facility.” In a statement at the time, its parent company, Vrable, said it was working with authorities. Arlington Court and Vrable did not respond to multiple requests for comment for this article.
Flushing of the pipes is critical anytime a building, or an area of a building, is not in regular use. Edens emphasizes the importance of water management strategies such as flushing water pipes, controlling temperatures and using disinfectant within a building. “We know water in the tap is not sterile,” he says. “The purpose of water management is to ensure that if some Legionella bacteria come through the main, the bacteria have nowhere to grow and hide.” He added that, under ideal conditions, Legionella can create a biofilm that helps it survive hot water and chlorine — another thing water management should aim to prevent.
Flushing of the pipes is critical anytime a building, or an area of a building, is not in regular use. And because Legionella bacteria rapidly reproduce at temperatures between about 75 ºF (24 ºC) and nearly 120 ºF (49 ºC), it’s also important to keep hot water hot and cold water cold.
Adding chlorine or other disinfectants to water as it enters a building is yet another tactic to reduce contamination. Chlorine, which is generally applied after filtration at a drinking water treatment plant, can drop to ineffective levels by the time water reaches the point of use. Supplemental chemical treatment such as a chlorine booster can bring disinfectant levels back within a range that limits Legionella growth.
Consumers can also take steps to reduce risks in their own households. For example, the CDC recommends that hot tub or spa owners frequently test water for proper levels of chlorine, bromine and pH. Old piping and “dead legs” — altered, abandoned or capped sections of pipe — can also provide the opportunity for Legionella to grow. And precautions should always be taken for stagnant water.
“You need to consider the far reaches of the building. If you’re not using a second bathroom, for example, then flush the shower before people use it,” says Cotruvo. “And don’t inhale while flushing.” Cotruvo also recommends using hot water regularly so water doesn’t stagnate in the pipes; maintaining hot water heater settings at about 130 ºF (54 ºC), blending hot and cold water at the tap to avoid scalding; and not spending excessive time in the shower or bathroom.
Regulatory Gaps
In a report published in August 2019 by the National Academies of Sciences, Engineering. and Medicine, a 13-member committee warned that current laws — even the SDWA — fail to protect the public from the spread of Legionella.
The authors, who include Rose and Pruden, lament that the bacterium is managed in water systems “on an ad hoc basis.” A handful of federal, state and local regulations require certain buildings to have water management plans that include monitoring for and treatment of Legionella. But no federal law targets Legionella contamination of water supplies and building water systems.
The committee offered several recommendations for improving Legionella management in the U.S., such as requiring a minimum disinfectant level throughout public water systems, developing clinical tools to capture more cases of Legionnaires’ disease, providing more guidance to homeowners, no longer allowing low-flow fixtures in hospitals and long-term care facilities, and addressing the longer periods of time that water sits idle and lower hot-water temperatures common in green buildings.
Pruden expresses hope that the document is a “point of reference for those motivated to take action,” but acknowledges today’s challenges: “There is also a great deal of political distraction and other issues getting priority.”
The EPA notes that it regulates Legionella in public water systems under the Surface Water Treatment Rule (SWTR), which is tied to the SDWA. The rule was originally written to control viruses and Giardia, then amended to control Cryptosporidium. The agency suggests that it is currently considering potential changes to requirements on disinfectant residuals and other measures that may provide for better control of Legionella in plumbing systems.
But many scientists argue a need for more urgent attention to and action on the issue.
For Legionella, the SWTR provides only “lip service” to the control of Legionella, says Rose. She suggests that disinfectant residual alone is inadequate to control the bacteria.
“We need some coordination at the [federal] level,” adds Pruden. “It’s a multi-stakeholder problem, but is now awkwardly being handled through the litigation system.”
Pruden highlights a serious roadblock to use of supplemental building-scale disinfectant: If a manager wants to proactively treat the water, according to strict interpretation of the SDWA, then the building effectively becomes a water system and is required to comply with EPA guidance on monitoring and testing.
“It becomes onerous, and creates a disincentive to do something about it,” says Pruden. She suggests that the EPA could amend the SDWA to eliminate this obstacle.
Tim Keane, a Philadelphia-area consulting engineer who focuses on Legionella control, also underscores the need for further regulatory and communication requirements to protect the public. In a paper published in September, Keane and researchers from Virginia Tech including Pruden detailed a 2015 Legionnaires’ disease outbreak in Quincy, Illinois.
While the initial outbreak investigation focused on the Illinois Veteran’s Home, where 58 people got sick and 12 died, some people in the community also acquired the disease without spending time in the veteran’s home. Keane found that a change in the primary disinfectant and an interruption in corrosion control several months before the outbreak resulted in a sustained drop in the level of disinfectant throughout the city’s distribution system. The municipal system deficiencies, the researchers wrote, “occurred in Quincy without any legal violations in the municipal water system or public acknowledgment of community-wide health risks.”
“This outbreak was similar to Flint in that a major change in city water quality issues resulted in an outbreak at a healthcare facility,” says Keane. “The huge difference was it occurred in Quincy without legal violations. So, outcomes as bad as Flint and Quincy can occur because of serious issues in our EPA regulations.”
A range of codes, standards and guidance documents have been sporadically adopted across the U.S. The CDC, for example, has published recommendations for buildings, including steps operators can take to reduce the growth and spread of Legionella. A free tool kit, as well as specific guidance for cooling towers and hot tubs, is available online, in addition to the agency’s guidance on reopening buildings.
Keane points to other documents, including from the Washington State Department of Health, that he says provide safer guidance for post-Covid building restarts.
Disinfection Considerations
Treatment considerations are further complicated by the other pathogens that can infiltrate U.S. drinking water systems. “It’s not just Legionella. Others live happily in the water,” says Caitlin Proctor, an assistant professor of agricultural and biological engineering and environmental and ecological engineering at Purdue University.
The environments in which these microorganisms flourish may differ. Proctor and Pruden are both studying how various organisms respond to different disinfectants. While one might work well against Legionella, Proctor notes, it could fail against non-tuberculosis mycobacterium, a relatively common menace in health-care settings. Overuse of disinfection is also a consideration: Disinfection chemicals can potentially produce unhealthy disinfection byproducts.
“Disinfection definitively saves lives,” Proctor says. “But we need to optimize the use and make the best choices.”
Disinfection could also raise the risk of antibiotic resistance. Genes that allow pathogens to survive disinfection could potentially confer resistance to antibiotics. It’s a hypothesis that warrants further investigation, according to Pruden.
“I view it as a worthy line of investigation to make sure our water treatments and mitigations are not making pathogens more antibiotic resistant,” adds Pruden. “We have a lot to be proud of over the last century in addressing fecal-born disease — cholera, typhoid. But the next frontier is not just treating the water but delivering safe water.”
Related Posts
Ensia shares solutions-focused stories free of charge through our online magazine and partner media. That means audiences around the world have ready access to stories that can — and do — help them shape a better future. If you value our work, please show your support today.
Yes, I'll support Ensia!




